Oral Presentation 1st Asia Pacific Herbert Fleisch Workshop 2025
Components of osteoporosis and long-term cardiovascular disease outcomes (#10)
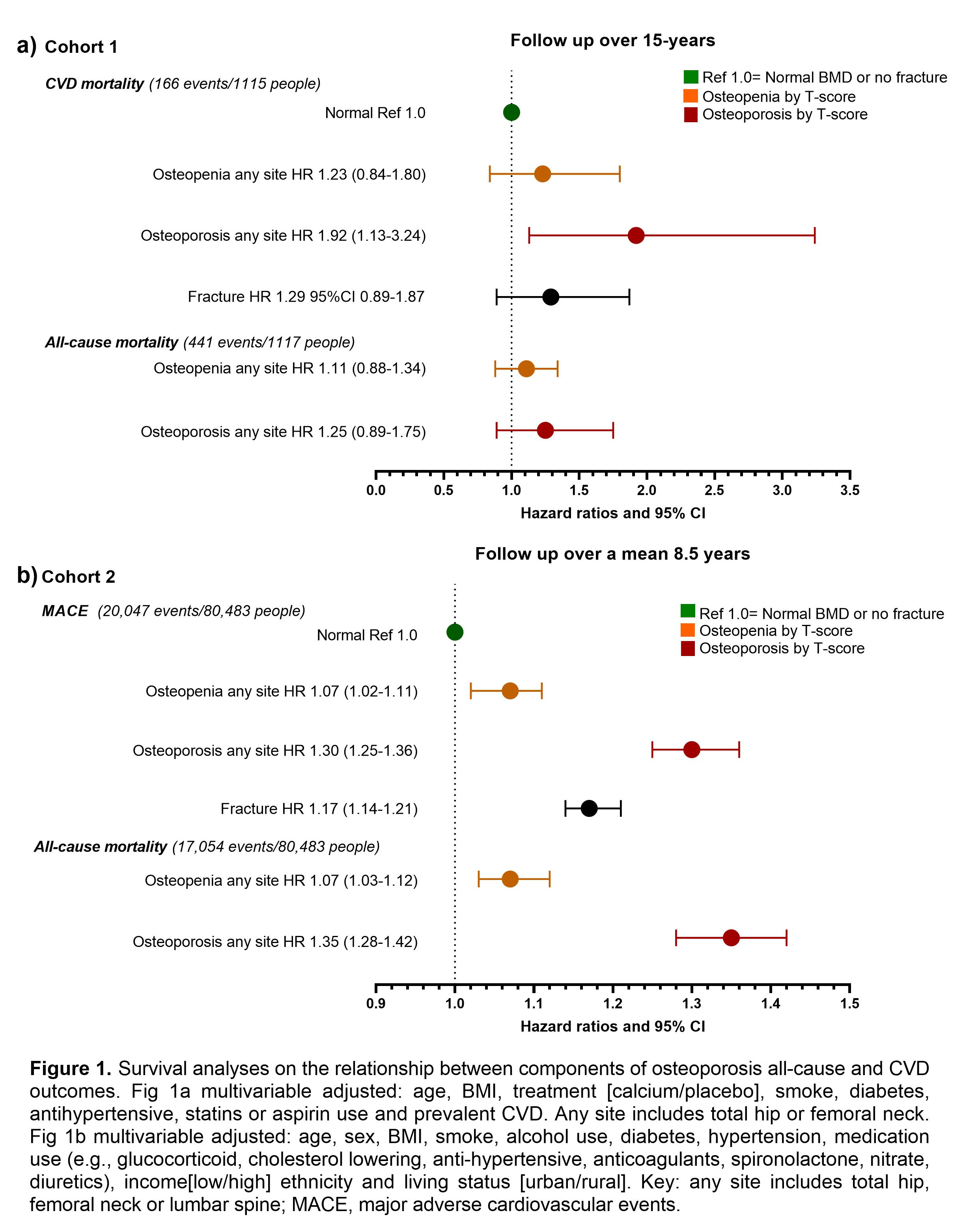
Aims: Osteoporosis has been linked to increased cardiovascular disease (CVD) risk. However, the long-term risk of CVD outcomes associated with components of osteoporosis (T-scores and osteoporotic fractures) remains unclear. We explored whether osteoporosis was associated with increased long-term risk of CVD mortality in 1,117 older women (cohort 1, mean±SD age of 75.0±2.6 years), then performed a replication study in a registry-based cohort of 80,483 people reflective of routine practice (cohort 2, 66.5±9.6 years, 94.7% female).
Methods: Bone mineral density (BMD) was assessed by dual-energy x-ray absorptiometry. Osteoporosis defined by a T-score of ≤-2.5 and osteopenia as T-score between -2.5 and -1.0. Mortality/event data obtained from linked health data. Models adjusted for CVD risk factors.
Results: In cohort 1, 59.7% had osteopenia at any site (total hip or femoral neck) and 27.7% had osteoporosis with 166 deaths (14.9%) over 15-years due to CVD. Compared to having normal BMD, osteoporosis at any site was associated with 92% increased risk for 15-year CVD mortality (Fig 1a). In cohort 2, 50.4% had osteopenia at any site (total hip, femoral neck or lumbar spine) and 25.4% had osteoporosis with 20,047 (24.9%) major adverse cardiovascular events (MACE) over 8.5 years. Compared with normal BMD, having osteoporosis at any site was associated with a 17-35% increase MACE and its outcomes, hospitalized acute myocardial infarction, ischemic cerebrovascular disease and all-cause mortality (Fig 1b). Regional differences were observed with a site-specific relationship with MACE, the strongest association was observed at the hip.
Conclusion: Osteoporosis, defined as low bone mineral density or previous fracture, is associated with higher long-term risk for CVD events. Further work is needed to identify whether this relationship is causal and to identify potential mechanisms. Low BMD may offer a novel strategy to screen for higher risk older women where CVD risk remains underrecognized.