Poster Presentation 1st Asia Pacific Herbert Fleisch Workshop 2025
Zoledronic Acid in Pediatric Acute Lymphoblastic Leukemia: A Case Report of Region-Specific Bone Recovery (#116)
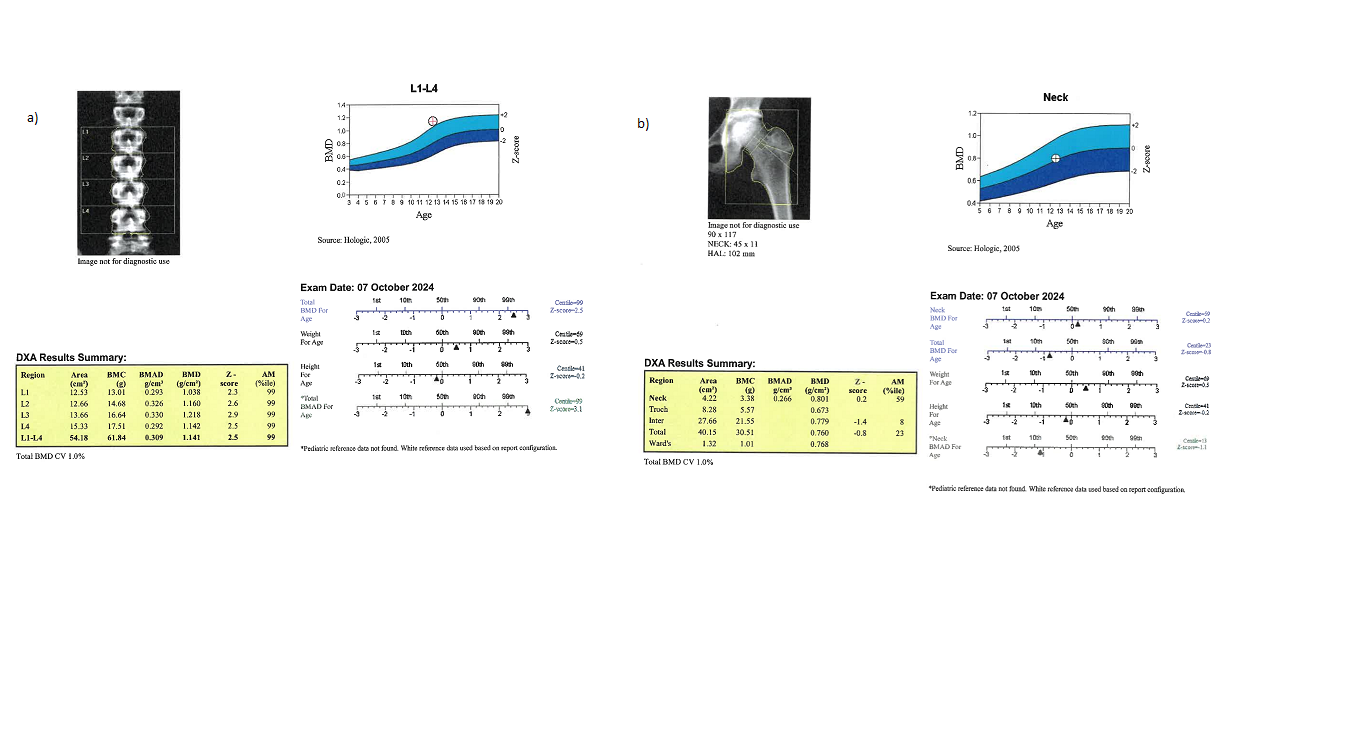
Skeletal morbidity is a common yet often under-recognized complication in children with acute lymphoblastic leukemia (ALL). Bisphosphonates are frequently used to manage skeletal complications in children with secondary osteoporosis; however, evidence on region-specific and long-term skeletal responses, particularly following zoledronic acid (ZA), a third-generation bisphosphonate, remains limited. We report the case of an 8-year-old girl with standard-risk ALL who developed vertebral fractures during maintenance chemotherapy and received a single intravenous dose of ZA (0.0275 mg/kg). Dual-energy X-ray absorptiometry (DXA) demonstrated a markedly elevated lumbar spine bone mineral density (BMD) (Z-score +2.60) at 1-year follow-up, which was sustained at 4-year follow-up (Figure 1a). In contrast, femoral neck BMD exhibited a delayed but progressive recovery, improving from a low Z-score of -3.40 to +0.20 at the 4-year follow-up (Figure 1b). Additional assessments using peripheral quantitative computed tomography (pQCT) and trabecular bone score (TBS) provided complementary qualitative insights. At four years post-ZA infusion, TBS was elevated (Z-score +1.40), and pQCT demonstrated markedly increased tibial cortical thickness (Z-score +1.73). At this timepoint, bone turnover markers were within normal pediatric reference ranges. This case illustrates the region- and time-dependent skeletal response to ZA in a pediatric oncology patient. It underscores the importance of site-specific imaging in long-term monitoring and highlights the limitations of systemic bone turnover markers in capturing localized skeletal changes. Until controlled trials become feasible, we propose that follow-up care for children receiving bisphosphonates incorporate imaging protocols that account for temporal and anatomical variability, including bone geometry and microarchitecture assessments.